Dry Eye Treatment

Dry Eye can have a major impact on your quality of life. You may find your eyes get tired faster or you have difficulty reading. Not to mention the discomfort of a burning sensation or blurry vision. Let’s take a look at dry eye treatments – from simple self-care to innovative prescriptions and therapies – to help you see clearly and comfortably.
What is dry eye disease (DED)?
Dry eye is a complex disorder characterized by insufficient tear production, poor tear quality overall, or excessive tear evaporation. It affects millions of people of all ages with a wide range of symptoms including eye irritation, light sensitivity, eye fatigue, watery eyes, fluctuations in vision, redness, burning, reduced contact lens wearing time, and more. This is a chronic condition that is typically progressive with episodes of flare ups.
What causes dry eye?
Arguably the biggest challenge with dry eye disease are the many factors that play a role in causing, contributing to, or aggravating dry eye. These include:
Most common medications groups
Antihistamines (allergies)
Decongestants
Antidepressants
Beta blockers and diuretics (high blood pressure),
Hormonal changes and medications
Antiacne
Analgesics (aspirin/ibuprofen)
Birth control
Glaucoma drops
And many more!
Past eye surgeries such as LASIK, PRK, and cataracts
Contact lens usage and overwear
Environmental factors
Extended computer use and/or reading significantly reduces our blink rate and the quality of our blinks
Dry air and changes in humidity
Systemic diseases associates
Rheumatoid arthritis, sjogrens disease, lupus, thyroid disease, rosacea,
Eyelid inflammations and malformations
Meibomian gland dysfunction (MGD) contributes to nearly 90% of all dry eye cases. There are glands that run radially inside both our upper and lower eyelids that express a small amount of lipid (oil) with each blink. This oil is critical in preventing evaporation of tears and helps keep them on the eyes longer. MGD occurs when the consistency of the oil becomes more dense, similar to a paste and the glands become blocked and difficult to express
Blepharitis and demodex are bacterial and mite infestations, respectively.
Lagophthalmos is when eyes do not close all the way when sleeping
Dehydration
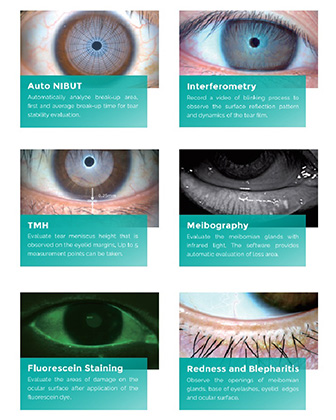
Diagnosing Dry Eye
Given the complexity of the disease, a thorough work-up dedicated to dry eye is critical as a baseline and to guide further treatment regimens accordingly. This includes:
Careful examination of eyelid structure and blink rate
Using special dyes to highlight any corneal abnormalities as well as the quality of the tear film
Measuring tear production
Assessing eyelid debris
Meibomian gland imaging and expression
Photos used each time to compare and adjust treatment regimen if necessary
Treatments we offer for Dry Eye
Artificial tears are used for comfort, however, do not address the underlying causes of dry eye
Oil-based preservative-free tears are what we recommend for daytime use
Gel drops are thicker and stay on the eye longer, which are ideal using before bed
Heated masks followed by expression
A healthy eyelid produces an oil which is key to helping tears stay on instead of evaporating away. A dry eye mask for 10 min followed by a gentle massage helps these express
Eyelid hygiene is critical in removing debris caked in the eyelashes, as well as bacterial biofilms along the lid margin
Eyelid wipes and sprays are available with particular ingredients necessary to decrease inflammation
Multiple types depending on the cause
Nutritional supplements with omega-3s are well accepted in improving dry eye symptoms and improving meibomian gland quality.
Short-term prescription management
For acute flare-ups, sometimes a steroid drop is required for 1-2 weeks with close monitoring to improve symptoms
Long-term prescription management
Restasis, Cequa, and Xiidra are eyedrops used twice daily that improve symptoms by decreasing inflammation and increasing quality of tears
Punctal Plugs
These are very tiny inserts placed in the eyelids that block the drainage channel of the tears. The helps keep more tears on the eyes and less drops to be used throughout the day. It is painless and takes less than one minute to perform in-office
Amniotic membranes
This is an allograft made through donor tissue that is placed on the eye and then covered with a contact lens on top. Over the course of 3-5 days, it slowly dissolves and then the contact is removed
This has many growth factors, anti-inflammatory and anti-scarring properties, which has shown to be significantly effective in treating corneal disease


